Mandrup-Poulsen Group - Immuno-endocrinology
Autoimmune and inflammatory endocrinopathies are non-curable diseases, and clinical management focuses on either hormonal substitution therapy or disease activity modification.
Substitution therapy of most hormonal deficiencies secondary to inflammatory endocrine tissue destruction is gratifying and restores normal life quality and expectancy.
Notable exceptions from these are type 1 and type 2 diabetes that are notoriously problematic to manage and are still associated with significant over-morbidity and mortality.
Therefore, these diseases present pressing needs for better causative treatments based on detailed insights into the molecular and cellular pathogenetic mechanisms.
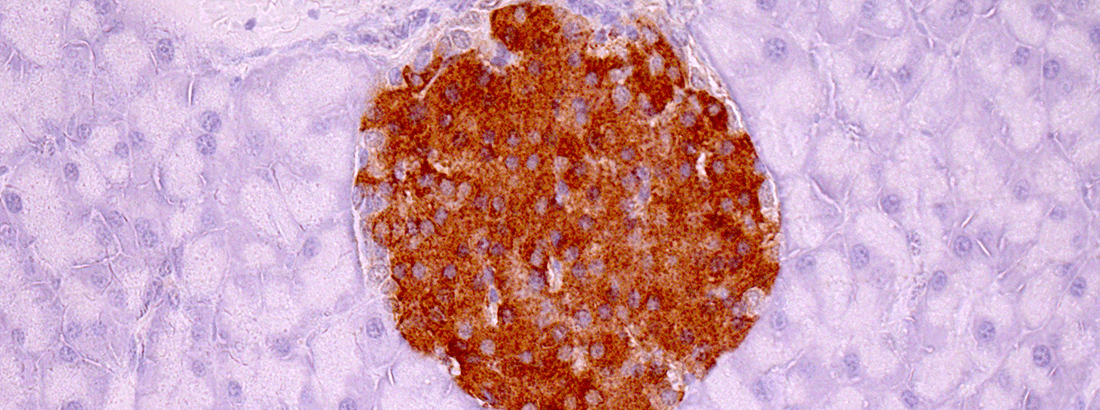
In our group, we aim to decipher such mechanisms, primarily focusing on pancreatic beta-cell dysfunction, a main driver of both type 1 and type 2 diabetes, and the cardiomyocyte with the perspective to identify novel therapeutic targets to improve treatment of these diseases and their cardiovascular complications.
The Immuno-endocrinology lab employs an interdisciplinary and collaborative research strategy to unravel transcriptional, translational and posttranslational responses to stress by two complementary approaches: a hypothesis-driven approach evolving from new discoveries in the lab, and an unbiased screening approach employing systems biology and using functional genomics, transcriptomics, proteomics, secretomics and post-translatomics.
Our experimental tactics utilise systems biology, bioinformatics, and in silico modelling, cell-free and cell-based in vitro models, ex vivo and in vivo studies in induced and genetic experimental animals, and clinical trials, epidemiological analyses and biomarker studies.
We employ amongst others the following laboratory techniques:
- islet isolation, culture, insulin secretion assays incl. perifusion
- cell-culture,
- viability, apoptosis and functional assays,
- gene expression (RT-qPCR),
- protein analysis (reducing and non-reducing SDS-PAGE, Western blotting, immunoprecipitation, protein expression systems, mass spectrometry, size-exclusion chromatography),
- gene knock-down or knock-out (siRNA, shRNA, CRISPR-Cas9),
- plasmid design,
- cloning, transfection,
- advanced imaging in collaboration with the Core Facility for Integrated Microscopy
- and many more, depending on the needs of the project
1) Metabolic and inflammatory regulation of the circadian clock: roles in the pathogenesis of diabetes and its cardiovascular complications.
Funded by the University of Copenhagen, the Novo Nordisk Foundation, Independent Research Fund Denmark, and the Danish Cardiovascular Academy.
Staff: Phillip Keller Andersen, MSc, PhD student; Rasmus Henrik Reeh, MD, PhD student, Emilie Bender, Master’s student, Isabel Sanders, Master’s student, Gayle Gajadin, Master’s student and Sussi Mørkeberg Kristoffersen, lab technician
Collaborators: Charna Dibner, University of Geneva, Switzerland; Zach Gerhart-Hines, University of Copenhagen; Frank Scheer, Brigham and Womens Hospital, Harvard Medical School, Boston, MA, USA;Louis Ptacek, University of California, San Francisco, CA, USA; Anne Helene Garde, NFA, Copenhagen; Christina Ellervik, Childrens’ Hospital, Harvard Medical School, Boston, MA, USA; Martin Young and Sethu Palaniappan, The University of Alabama at Birmingham, AL, USA.
Prolonged perturbation of the circadian clock is associated with detrimental metabolic outcomes and a risk factor for obesity and cardiometabolic diseases. There is increasing interest in understanding the mutual interplay between the circadian clock and metabolic/inflammatory responses. The hypothesis of these projects is that metabolic and inflammatory stressors perturb the islet and cardiomyocyte circadian clock, and that clock perturbation sensitizes these cells to damage. We have recently discovered that high glucose and/or free fatty acid concentrations and inflammatory cytokines lead to distinct aberrant regulations of key clock components in insulin-producing cell lines, and we now wish to confirm and extend these observations in other model systems, as well as disentangle the molecular mechanisms.
2) Targeting mitophagy to prevent beta-cell failure in Type 1 Diabetes
Funded by the Juvenile Diabetes Research Foundation USA, with the University of Michigan Medical School, the Sehested-Hansen Foundation and the Independent Research Fund Denmark.
Staff: Jette Bach Agergaard, MSc, PhD student; Sussi Mørkeberg Kristoffersen, lab technician.
Collaborators/Co-supervisors: Scott Soleimanpour, University of Michigan, USA; Clara Pratts, Core Facility for Integrated Microscopy, University of Copenhagen
Type 1 Diabetes (T1D) results from autoimmune-mediated beta-cell damage leading to insufficient functional beta-cell mass to meet peripheral insulin demands. Beta-cells rely upon mitochondrial respiration to generate the energy necessary for insulin synthesis, processing, and secretion. Immune-mediated cytokine release also leads to generation of intracellular reactive oxygen species and mitochondrial damage, which ultimately result in beta-cell apoptosis. Indeed, defects in mitochondrial structure and function have been reported in beta-cells of patients with both T1D and T2D. Defects in mitochondrial structure and function are characteristics of impairments in mitophagy, a selective form of autophagy necessary for elimination of dysfunctional mitochondria; however, the role of mitophagy in T1D pathogenesis is not well understood. Our collaborators at the University of Michigan (PI Scott Soleimanpour) previously discovered a key role for the T1D susceptibility gene Clec16a in control of glucose homeostasis in humans and mice through its regulation of beta-cell mitophagy. Therefore, our goal is to dissect the mechanistic and physiologic regulation of Clec16a-mediated mitophagy in beta-cells to elucidate its contribution to T1D pathogenesis.
3) Genetic conditions of insulin hypersecretion as models of endoplasmic reticulum stress, beta-cell ageing and Type 2 Diabetes.
Funded by the Novo Nordisk Foundation and Independent Research Fund Denmark. This project is spear-headed by Postdoc Anniek Lubberding who runs her own sub-group within the Immuno-endocrinology lab.
Staff: Anniek Lubberding, MSc, PhD, postdoc; Emil Zeng Skovhøj, MSc, PhD student; Mathilde Sonne Søndergaard, MSc, Research assistant; Wen Han, Roekaya Djorai & Vanessa Zeidler, Master’s students; Sussi Mørkeberg Kristoffersen, lab technician.
Collaborators: Thomas Jespersen, Signe Torekov, Jørgen Kanters, Jonas Treebak, Torben Hansen, University of Copenhagen; Dr. Sebastian Barg, Uppsala University; Prof. Patrik Rorsman, University of Oxford; Dr. Andrei Tarasov, Ulster University; Dr. Bjørn Tyrberg, Servier; Dr. Sif Groth Rønn, Novo Nordisk; Professor Patrick MacDonald, University of Alberta.
Type 2 Diabetes (T2D) arises when beta-cell insulin secretion fails to meet insulin demands, typically due to insulin resistance as a consequence of obesity. A polygenetic disposition sets the threshold for at what level of secretory demand decompensations occurs. Since the risk of decompensation increases with age, it is important to understand how the gene-age interaction affects insulin biosynthesis, handling and secretion.
As secretory demand increases the handling of proinsulin in the endoplasmic reticulum (ER), the ER becomes a limiting factor for insulin biosynthesis and secretion. This handling mismatch may eventually trigger the unfolded protein response and ER stress, known to activate proinflammatory and proapoptotic pathways in turn impairing beta-cell function and viability. The Akita mouse model carrying a mutation in the proinsulin-2 gene is proof of principle for this hypothesis.
We study other genetic models with human relevance that affect insulin secretion to clarify the molecular mechanisms underlying beta-cell failure in ageing.
The Immuno-endocrinology lab is supported by grants from a number of private and public foundations. Listed below is a selection of public and private funds the group has received in the last years
Independent Research Fund Denmark
European Foundation for the Study of Diabetes and Lilly European Diabetes Research Programme
(EFSD/Lilly Programme)
Bjarne Jensens Fond (Danish)
Kirsten og Freddy Johansens Fond (Danish)
Poul og Erna Sehested Hansens Foundation
Dagmar Marshall Fond
Vera & Flemming Westerberg Foundation
Prins Bernhard Cultuurfonds
Research education
The Immuno-endocrinology lab prioritises research-based teaching by taking responsibility for pre- and postgraduate courses, as well as practical research training of our Bachelor’s, Master’s and PhD students, as well as Postdocs and Visiting Scientists.
Training in our lab
Aside from practical training in the lab, all lab members are encouraged to participate in fundraising, manuscript writing, scientific reviews, academic assessments, research administration and intra- and extra-mural committee work and to contribute actively and positively to group, section, department, faculty and university activities.
The dissemination policy of the Immuno-endocrinology lab
The Immuno-endocrinology lab is careful to secure intellectual property rights via patenting and priority publication in high-rank international periodicals.
Furthermore, we are passionate about data sharing via public databases and dissemination of research findings to the broader public by press releases, presentations at scientific and public meetings, in patient organisations and in the media.
We are looking for highly motivated Master's students to work with us on all projects listed under Research Projects, although availability may vary over time. Additionally, pilot or new projects may be available at times.
The overall aim of the current research portfolio of the Immuno-endocrinology lab is to identify novel therapeutic targets in the pathways leading to diabetes and its complications with a focus on responses to immune, inflammatory, metabolic, ageing- related and oxidative stressors.
Our translational experimental strategy is to move from cell-lines to primary to human tissue experiments, the latter mainly used to confirm critical observations from cell lines and rodent tissues. Studies also involve animal, clinical and epidemiological studies.
The projects involve PhD, Master’s, Bachelor’s and ERASMUS students with a close and direct supervision and coaching from postdocs and tenured faculty members. They encourage independence from the start and the opportunity to learn about the diverse aspects of science: literature search, experimental design, experimental planning and execution, data-analysis and -presentation, interaction with our collaborators as well as grant-writing and active participation in administrative and social aspects of faculty, laboratory and group life.
PhD students are involved in undergraduate teaching and offered mentoring of Bachelor’s or Master’s students in their senior years.
Students will have the opportunity to learn following techniques:
- islet isolation,
- cell- and islet-culture,
- viability and functional assays, e.g. glucose-stimuated insulin release and islet perifusion to determine 1st and 2nd phase insulin secretion
- gene expression (RT-qPCR),
- protein analysis (reducing and non-reducing SDS-PAGE, Western blotting, immunoprecipitation, protein expression systems, mass spectrometry, size-exclusion chromatography),
- gene knock-down or knock-out (siRNA, shRNA, CRISPR-Cas9),
- plasmid design,
- cloning, transfection,
- pancreatic islet handling and usage
- advanced imaging
- and many more, depending on the needs of the project
Group members
| Name | Title | Phone | |
|---|---|---|---|
| Rasmus Henrik Reeh | Research Assistant | +4535333848 | |
| Thomas Mandrup-Poulsen | Professor | +4535327254 |
Group Leader
Thomas Mandrup-Poulsen
Professor
Phone: +45 3033 0387
tmpo@sund.ku.dk
ORCID: 0000-0002-3215-9273

